A mother has urged all pregnant women to take the whooping cough jab after her newborn spent 10 days in a coma with the infection.
Polly Deehy, from Dartford, Kent, was an otherwise healthy baby until her terrifying ordeal.
In April, at just two weeks old, she developed a rattly cough that left her struggling to breathe.
She was rushed to hospital four days later by her parents when she suddenly turned blue, her mother Kerry Pearson revealed.
After her condition worsened she was transferred to St Mary’s Hospital in London where medics diagnosed her with pertussis, nicknamed the ‘100-day cough’, and put her on a ventilator.
Polly’s story and Ms Pearson’s warning comes amid a worrying surge in cases which has already killed five babies. Experts have already warned the outbreak could be the biggest for 40 years.

Polly Deehy, from Dartford, Kent, was an otherwise healthy baby until her terrifying ordeal. In April, at just two weeks old, she developed a rattly cough that left her struggling to breathe. She was rushed to hospital four days later by her parents when she suddenly turned blue, her mother Kerry Pearson (pictured) revealed

After her condition worsened she was transferred to St Mary’s Hospital in London where medics diagnosed her with pertussis, nicknamed the ‘100-day cough’, and put her on a ventilator

Ms Pearson had a whooping cough vaccine when she was a child, and again during her pregnancy with her son, now seven. But the 26-year-old has claimed she wasn’t offered the vaccine when pregnant with Polly
Yet as a few as a quarter of expectant mothers have had the pertussis jab – offered between 16 and 32 weeks — in parts of London.
The jab protects babies in the first few months of their life, when they are most vulnerable and before they can receive their own vaccines.
Ms Pearson had a whooping cough vaccine when she was a child, and again during her pregnancy with her son, now seven.
But the 26-year-old has claimed she wasn’t offered the vaccine when pregnant with Polly.
She said: ‘I knew nothing about whooping cough — it was just something from my grandparents’ era.
‘There’s no treatment and no cure, we’re just having to wait and it’s unbearable.
‘If I’d had the vaccine during my pregnancy I’d have passed on the antibodies in my breastmilk.
‘The vaccine should be routinely offered with every pregnancy.
‘I just want people to be aware, you should have the whooping cough vaccine when you’re pregnant.’
She added: ‘If you’re not offered it then please demand it.
‘If you’re an anti-vaxxer please reconsider — this is deadly to infants — it’s not worth the risk.
‘Nothing is worth going through what we’re going through.’
Almost 3,000 whooping cough cases have already been recorded in 2024 — triple the levels seen across the entirety of 2023.

Polly was born on March 26 after an uncomplicated labour (pictured with Mum Ms Pearson and Dad Jack Deehy, 29) and was returned home the very same day. Just four days later, however, Ms Pearson, experienced chills, a headache and very rattly cough. By April 6, Polly had developed the same symptoms
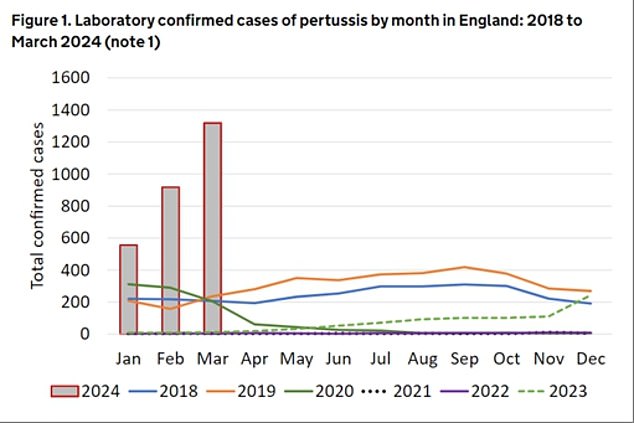
Almost 3,000 cases have already been recorded in 2024 — triple the levels seen across the entirety of 2023. Health chiefs say Covid lockdowns have fuelled England’s unprecedented pertussis epidemic, nicknamed the ‘100-day cough’
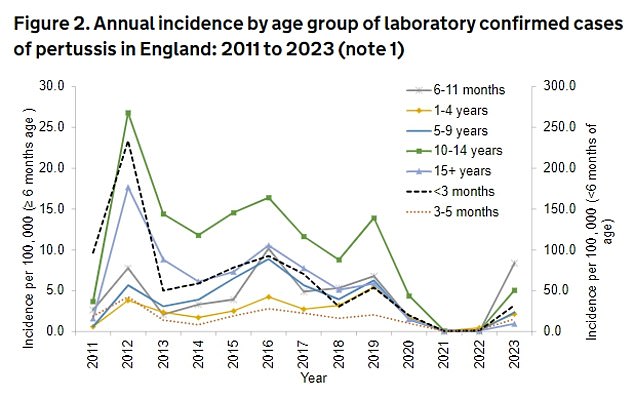
Over half (50.8 per cent) of all whooping cases in 2024 have been among those aged 15 and older, with more than a quarter (28.6 per cent) in children aged 10 to 14. But the rates of whooping cough remained highest in babies under three months, UKHSA noted
Five babies have died so far this year. All were under the age of three months.
Vaccination rates have also slumped in the wake of the pandemic in a trend experts blame on growing jab scepticism.
Polly was born on March 26 after an uncomplicated labour and was returned home the very same day.
Just four days later, however, Ms Pearson, experienced chills, a headache and very rattly cough.
By April 6, Polly had developed the same symptoms.
After she was rushed to hospital by she was put on a paediatric ward on an oxygen-flow machine, which provided extra oxygen for her to breathe.
But she kept turning blue as her oxygen levels plummeted, and her breathing kept stopping.
On April 13, she was transferred to St Mary’s Hospital and immediately put on a ventilator in an induced coma.
Tests for whooping cough came back positive the next day.
Polly was slowly taken off the life-support and is now able to breathe independently.
She was woken from her coma on April 22, and came out of the intensive care unit on April 24.
Ms Pearson said: ‘I’ve never been more relieved in my life. I watched them take the tubes out and turn all the machines off [as she recovered]. It was the best thing ever.
‘The odds were not in her favour, but she’s been very very lucky. There’s no evidence of any lasting problems, but she might have a bit of weakness in her lungs — time will tell.’
She added: ‘We caught it in time so she was in hospital, but if she’d had those blue episodes at home she’d have suffered lasting damage because of the lack of oxygen.
‘We need to educate people about the vaccine and the symptoms.
‘Whooping cough is dangerous to newborns and I want people to know what to look out for.’
Dozens of babies died each year before the pregnancy jab roll-out was introduced in England in 2012.
Only 21 fatalities were recorded between then and 2023. All but two of their mothers were unvaccinated.
MailOnline understands of the five babies who have died in 2024 — all under the age of three months — two of their mothers were unvaccinated.
Less than two thirds (59.5 per cent) of expectant mothers in England took the pertussis vaccine, latest figures for 2023 show.
Uptake of the six-in-one jab — offered to babies in their first couple months of life — is also at an all-time low.
Just 91.8 per cent were fully vaccinated by their 1st birthday in 2022/23, according to NHS figures.
Babies are given three doses of the six-in-one jab at eight, 12 and 16 weeks of age to protect against whooping cough and other serious diseases such as diphtheria and polio.
A pre-school booster is offered after they turn three.
Experts are desperately trying to ramp up vaccination rates, pleading with mothers-to-be to get jabbed.
Dr Gayatri Amirthalingam, consultant epidemiologist at UK Health Security Agency (UKHSA), said: ‘Vaccination remains the best defence against whooping cough and it is vital that pregnant women and young infants receive their vaccines at the right time.
‘Whooping cough can affect people of all ages but for very young babies it can be extremely serious.’
Dr Michael Head, senior research fellow in global health, University of Southampton, said: ‘Whooping cough can and does kill babies.
‘A high coverage of vaccination is vital in reducing transmission within populations.
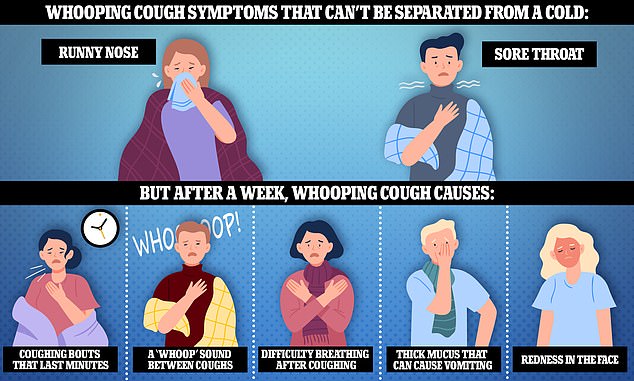
Health officials warned that the infection is initially difficult to tell apart from a cold, as the first signs are a runny nose and sore throat. But around a week later, sufferers may develop coughing bouts that last minutes, struggle to breathe after coughing and make a ‘whoop’ sound between coughs. Other signs of whooping cough include bringing up a thick mucus that can cause vomiting and becoming red in the face
‘Vaccine uptake in young children and for expectant mothers during pregnancy is so important. The vaccine is safe, and extremely effective.’
Professor Sir Andrew Pollard, consultant paediatrician and chairman of the Joint Committee on Vaccination and Immunisation, which advises the Government, today added: ‘The troubling thing is that if we continue to have high rates of spread and low rates of vaccination, there will be more babies severely affected and sadly there will be more deaths.’
Whooping cough can initially be difficult to tell apart from a cold, with the first signs typically being a runny nose and sore throat.
But around a week later, sufferers may develop coughing bouts which last minutes, struggle to breathe after coughing and make a ‘whoop’ sound between coughs.
Other signs of pertussis include bringing up a thick mucus that can cause vomiting and becoming red in the face.
Whooping cough is a cyclical illness which typically peaks every five years. The last occurred in 2016, when almost 6,000 cases were confirmed.
Pre-pandemic, between 2,500 and 4,500 suspected cases were logged each year. This fell to around 500 during the coronavirus crisis.
Lockdowns stifled the spread of pathogens as people met less.
UKHSA bosses said the impact of the Covid pandemic also means there is reduced immunity in the population. Similar rebounds were seen for flu and RSV.
Surveillance statistics show 2,793 lab-confirmed cases have been reported this year to the end of March.
Of these, 556 were logged in January, 918 in February and 1,319 in March.

Pregnant women are being urged to get the vaccine to protect their baby from catching the infection in the first few weeks of their life. Protection should last until they are old enough to get vaccinated themselves
Half (50.8 per cent) were among those aged 15 and older, with more than a quarter (28.6 per cent) in children aged 10 to 14.
But rates remained highest in babies under three months, who are most at risk.
However, infection rates are still nowhere near the annual high of 170,000 logged in the 1940s.
Routine vaccination, introduced in the 1950s, dramatically slashed levels.
Whooping cough is caused by the pertussis bacteria and is spread by coughing and sneezing.
Sufferers are infectious from around six days after cold-like symptoms begin to three weeks after their cough starts.
Doctors dish out antibiotics as treatment if the whooping cough is detected within three weeks.
However, if a person has been infected for longer, antibiotics will not speed up their recovery.
Whooping cough is less severe in older children and adults but can still cause sore ribs, a hernias, ear infections and urinary incontinence among these groups.










