Britain’s first three-parent baby has been born using a groundbreaking IVF procedure.
In the biggest leap forward since IVF itself, the technique, called mitochondrial donation treatment (MDT), protects children from a group of mitochondrial disorders, including muscular dystrophy, which can cause poor growth, muscle weakness, learning disabilities and early death.
These illnesses are inherited through faults in the mother’s mitochondria – the tiny ‘engine rooms’ which power the cells.
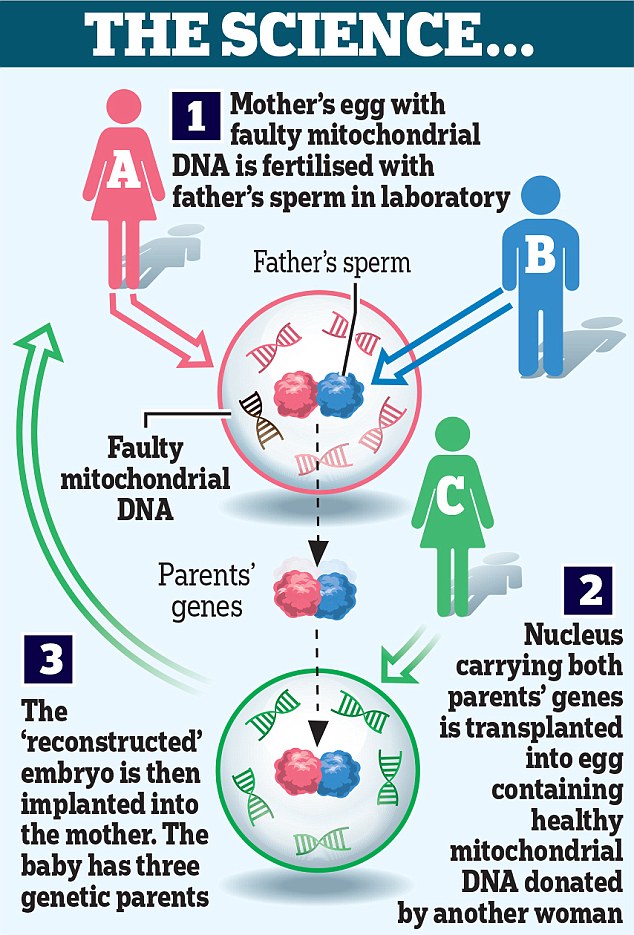
The MDT procedure allows women to swap their diseased mitochondria for the healthy mitochondria taken from the egg of a second woman.
The first ‘three-parent babies’ have been born using the technique, it was revealed in a Freedom of Information response provided to the Guardian by the UK’s fertility regulator, the Human Fertilisation and Embryology Authority (HFEA).
British scientists devised the new IVF technique, in which the child has genetic material from three people, but does not inherit any of the donor’s characteristics. Opponents include the Church of England

Britain’s first three-parent baby has been born using a groundbreaking IVF procedure

The babies will technically have two mothers but the second ‘mother’ in each case will have no real genetic link to the child. Pictured: File image of man and woman holding newborn baby
While the babies will technically have two mothers, the second ‘mother’ in each case will have no real genetic link to the child, contributing only 0.1 per cent of her DNA.
Critics have previously expressed fears the successful use of the technique could pave the way for ‘designer’ babies.
But supporters say mitochondrial donation is a lifeline for up to 3,000 women in danger of passing on potentially deadly diseases.
The HFEA confirmed that a small number of babies have now been born in the UK after MDT.
It has not provided an exact number, but said the number was ‘less than five’ as of April.
The families involved have not been identified, but the first three-parent babies could have been born to two mums who knew each other, with eligible women understood to have asked friends to be egg donors.
Sarah Norcross, director of the Progress Educational Trust (PET), a charity which campaigns to help people affected by genetic conditions and infertility, said: ‘The first baby born by a new technique is aways big news but a cautious reaction is particularly appropriate in this case.
‘For the time being, the HFEA only gives permission for mitochondrial donation to be used on a case-by-case basis.

Critics have previously expressed fears the successful use of the technique could pave the way for ‘designer’ babies
‘This is sensible, as it is still early days for this technology, and it needs to be monitored closely and carefully.’
Britain became the first country in the world to legalise three-parent babies under licence in 2015.
The Newcastle Fertility Centre at Life clinic was then given the green light to perform the procedure by the HFEA in 2017, in what was hailed as a ‘momentous day’.
Three-parent babies, using slightly varying methods, have already been born in countries including Mexico and Ukraine.
Controversially, it has been used abroad not only to prevent mitochondrial diseases being passed on, but as a method claimed to help an infertile woman conceive by using a second woman’s DNA.
British experts have said there is no evidence suggesting mitochondrial donation could work for this purpose.
The technique, used in this country to prevent mitochondrial disease only, removes the nucleus from the mother’s egg and puts it in an emptied-out egg donated by another woman.
But it is not without risk, and some experts are concerned moving the genetic material from one egg to another could affect the way in which the genes are expressed.

There are some concerns that the new technique could disrupt gene sequences leading to later health problems such as cancer or diabetes
Disrupting the activity of genes might produce a child at increased risk of later health problems, such as cancer or diabetes.’
Peter Thompson, chief executive of the HFEA, said: ‘Mitochondrial donation treatment offers families with severe inherited mitochondrial illness the possibility of a healthy child.
‘The UK was the first country in the world to allow mitochondrial donation treatment within a regulatory environment.
‘The HFEA oversee a robust framework which ensures that mitochondrial donation is provided in a safe and ethical manner.
‘All applications for treatment are assessed on an individual basis against the tests set out in the law and only after independent advice from experts.
‘These are still early days for mitochondrial donation treatment and the HFEA continues to review clinical and scientific developments.’










